Decoding The Immune Synapse To Create Novel Immunotherapies
By Anthony J. Coyle, PhD, President of Research and Development, Repertoire Immune Medicines
The COVID-19 pandemic has generated widespread interest in the immune system, not only in understanding its role in controlling SARS-CoV-2 infections, but also related to an increasing appreciation for the central role of immunology in health and disease.
Most of the recent attention has been focused on humoral immunity, which is the part of the adaptive immune system through which antibodies recognize and neutralize extracellular pathogens in order to fight a disease or protect against it. In one example, current COVID-19 vaccines are designed primarily to elicit neutralizing antibodies, which prevent virus binding and entry into cells. However, the adaptive immune system includes another essential component termed cell-mediated immunity. It relies on specialized cell types, primarily antigen-specific T cells, to orchestrate a wide range of immune system responses to disease-related antigens.
Through their T cell receptors (TCRs), T cells recognize peptides derived from a vast space of intracellular antigens. Successful antigen recognition then activates T cells to kill pathogen-infected or cancer cells, or to produce pro-inflammatory cytokines, such as interferons or interleukins. While antibodies mainly neutralize extracellular antigens and can wane relatively soon after a disease has resolved, T cells kill pathogen-infected or cancer cells and provide long-lasting protection through generation of T cell memory. Indirectly, T cells are also critical for the formation of optimal humoral responses.
Decades of research into cell-mediated adaptive immunity has led to groundbreaking modern medicines, such as checkpoint therapies for cancer, or disease modifying drugs that converted previously debilitating autoimmune diseases into managed chronic diseases. However, many of these drugs non-specifically modulate the immune system, causing sometimes severe side effects, such as autoimmunity for checkpoints or infections for immunosuppressants. It is only in recent years that we have developed the tools and technology needed to decode specific disease-relevant TCRs and antigens whose pharmacologic modulation is expected to yield selective immune therapies without the limitations of strategies addressing cell-mediated immunity.
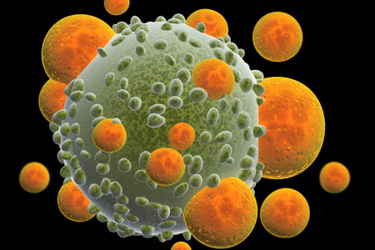
A key mechanism that determines cell-mediated immunity is the immune synapse, the molecular interface through which a T cell interacts with an antigen-presenting cell (APC). APCs process intracellular antigens, including viral proteins, load them onto major histocompatibility complex (MHC) proteins and display or present the resulting peptide-MHC complexes on the cell surface. Among the billions of T cells with different TCRs in a human, there are some that express the right TCRs, which recognize a specific peptide bound to a specific MHC protein. Binding of the right TCR to the peptide-MHC complex then initiates the formation of an immune synapse. It is this interaction that governs the behavior of the T cell.
The full repertoire of TCR-antigen interactions at the immune synapse is extraordinarily diverse. The reason is that across human populations, about a quadrillion different TCRs are juxtaposed to about a quadrillion different peptides and thousands of different MHC proteins. Combined with the exquisite specificity of individual immune synapses, this diversity gives us our own “immune security” because it makes sure that some T cells react with and control almost any pathogen or cancer cell we encounter. In uncontrolled disease, including cancer, this immune security is broken and the T cell repertoire perturbed.
By enabling us to restore immune security, the enormous repertoire of TCR-antigen codes presents one of the greatest opportunities in medical science for treating many diseases. However, despite the great therapeutic promise cell-mediated immunity holds, the translation of insights from cellular immunity to the development of new therapies has been limited by our inability to unveil the full diversity and complexity of the T cell repertoire. Thus, the ability to decipher immune synapses at scale is much needed.
Repertoire’s proprietary DECODE platform does just that: it allows us to decipher all aspects of the immune synapse and thereby understand the immune codes responsible for protecting us from disease. This “full decoding” of the immune synapse is the foundation for the company’s development of T cell therapies that harness the power of the individual’s own immune system to treat cancer, infectious diseases, autoimmune disorders, and other serious diseases.
Breaking the Code
Deciphering the complexity of the immune synapse and the cellular immunity that arises from it has been a major roadblock in the past. Repertoire’s DECODE platform overcomes this obstacle with four complementary technologies, each contributing part of the solution to deciphering the multiple elements of the immune synapse:
- MEDiTM, a mammalian epitope display platform that determines which peptides within an antigen can be presented across many different MHC proteins.
- MCRTM, an MHC-TCR fusion protein reporter technology, enables screening of T cell reactivity to vast numbers of peptides presented in the context of a wide and diverse set of MHC molecules.
- CIPHERTM, a technology that can screen millions of individual T cells and determine their peptide-MHC reactivity as well as their molecular phenotype and function.
- CAPTANTM, a suite of deep-learning computational tools that predict TCR reactivity and leverage data from the other three technologies.
Together, the technologies of Repertoire’s DECODE platform provide a comprehensive understanding of the immune synapse to date, and allow us to discover novel antigen epitopes and the phenotypes of the specific T cells they activate. We then apply that knowledge to the creation of novel, autologous T cell therapies with the intent to restore the patient’s own immune security.
Arming Autologous T cells Against Cancer
When considering therapies based on the TCR-antigen repertoire, it is easy to fall into the trap of thinking that those therapies are personalized. We study the TCR-antigen repertoires in specific populations of patients. For example, in patients with melanoma, we identify a set of antigens expressed on the many different patients’ tumors. We then develop peptides that correspond to these antigens in an off-the-shelf manner to train T cells isolated from the patient to have specificity for melanoma tumor cells. With this approach, we can generate autologous, multiclonal antigen-specific T cells that can be frozen and used for multiple administrations in the same patient.
These T cell products have three important features that contribute to their therapeutic effectiveness:
- First, they are multiclonal in nature, because the product contains T cells that respond to multiple antigens instead of just one. This leads to greater efficacy and a more durable response, and also reduces the likelihood of immune evasion by the tumor – all because the T cells can attack the tumor on multiple fronts.
- The second feature, which is unique, is that our T cell products can recognize and target multiple intracellular antigens that are presented on the cancer-cell surface by MHC proteins. This contrasts with CAR T cell therapies, which can recognize and target only surface antigens, usually in an MHC-independent manner, and with TCR-T cell therapies, which can recognize and target only a single MHC-presented peptide.
- Third, we can enhance the armamentarium of these multiclonal, antigen-specific T cells by attaching cytokines to their surface.
These characteristics enable us to use our nanogel technology to attach interleukin-15 (IL-15), which is designed to induce the proliferation and increase the survival of our T cells after infusion onto the patient and – importantly – prevents their exhaustion, thereby improving durability. Alternately, we can attach IL-12, a very potent activator of T cells; dendritic cells, which are important APCs; and natural killer cells, whose severe toxicity has prohibited systemic use of IL-12. But when attached to T cells, IL-12 is delivered only to the tumor microenvironment, where it unleashes the power of other immune cell types to give T cells an even greater tumor-killing effect while reducing or avoiding the systemic toxicity of IL-12.
Taking the Code Beyond Cancer
While T cell therapies have naturally attracted much attention for their potential in treating cancer, the DECODE platform has additional important applications in infectious diseases and autoimmune disorders such as type 1 diabetes (T1D), multiple sclerosis (MS), and other neuroimmunologic diseases.
As described above, we generate T cells for cancer based on our knowledge of the specific antigens that drive the strongest antitumor T cell responses. We can take this same approach to develop multiclonal, antigen-specific T cells that target and eliminate viruses. This approach could be particularly beneficial for transplant and other immunocompromised patients, in whom certain viral infections that are typically asymptomatic in immunocompetent individuals – such as cytomegalovirus (CMS) and Epstein-Barr virus (EBV) – are potentially dangerous and even life-threatening.
The application of DECODE in autoimmune diseases takes a somewhat different route by harnessing the power of T regulatory cells (Tregs), which ordinarily help maintain immune homeostasis and tolerance to self-proteins by dampening inappropriate T cell responses.
There have been only a few studies of Tregs in autoimmune diseases, most of which used expanded, polyclonal Tregs from the periphery whose specificities were unknown and which had little efficacy. However, we have learned that a Treg specific for a single antigen is a better suppressor than polyclonal Tregs. Thus, if we can determine the antigen underlying an autoimmune condition, then we can generate a Treg product that expresses the TCR for that antigen and treats the disease.
Indeed, with DECODE we can decipher the specificity of Tregs to enable the creation of multiple autoimmune disease therapies that are not broadly immunosuppressive but instead are designed to restore immune balance in these patients.
The potential of T cell therapies to be curative by harnessing our own immune repertoire has exciting implications for cancer and many other immune-mediated disorders. But the lack of understanding of that repertoire, and how it shapes T cell reactivity and function, can pose significant barriers to developing the most effective cell therapies. DECODE surmounts that barrier by delivering comprehensive and unique insights into the immune synapse, which we believe enables us to create the best possible T cell therapies for many patients with serious diseases.
Anthony J. Coyle, PhD, President of Research and Development, Repertoire Immune Medicines
 Tony is a biotech entrepreneur and renowned immunologist, with more than 25 years of experience in drug discovery and development, spanning academia, early-stage biotechnology companies and global pharmaceutical organizations. Prior to Repertoire, he was the Co-Founder, President and CEO of Pandion Therapeutics, a clinical-stage biotechnology company focused on developing novel bi-specific antibody therapeutics to locally modulate the immune system in a number of autoimmune disorders. Prior to Pandion, Tony was a Senior Vice President and Chief Scientific Officer at Pfizer, where he launched Pfizer’s Centers for Therapeutic Innovation (CTI), a collaborative Research and Development model between Pfizer and premier academic medical centers, patient advocacy groups and the National Institute of Health. Before Pfizer, he was Vice President and Global Head of Respiratory, Inflammation, and Autoimmunity Research at Medimmune Biologics, a Division of AstraZeneca. Tony also has held leadership positions at Millennium Pharmaceuticals and Glaxo Institute in Geneva.
Tony is a biotech entrepreneur and renowned immunologist, with more than 25 years of experience in drug discovery and development, spanning academia, early-stage biotechnology companies and global pharmaceutical organizations. Prior to Repertoire, he was the Co-Founder, President and CEO of Pandion Therapeutics, a clinical-stage biotechnology company focused on developing novel bi-specific antibody therapeutics to locally modulate the immune system in a number of autoimmune disorders. Prior to Pandion, Tony was a Senior Vice President and Chief Scientific Officer at Pfizer, where he launched Pfizer’s Centers for Therapeutic Innovation (CTI), a collaborative Research and Development model between Pfizer and premier academic medical centers, patient advocacy groups and the National Institute of Health. Before Pfizer, he was Vice President and Global Head of Respiratory, Inflammation, and Autoimmunity Research at Medimmune Biologics, a Division of AstraZeneca. Tony also has held leadership positions at Millennium Pharmaceuticals and Glaxo Institute in Geneva.
Tony has authored more than 200 peer-reviewed publications and holds 13 issued U.S. patents and more than 30 published patent applications. He speaks globally on his research and on collaborative approaches to drug development, and he served on the Scientific Advisory Boards of Children’s Hospital Boston Technology Development Fund and the Lupus Research Alliance in New York.
A graduate of King’s College, University of London, Tony was a postdoctoral fellow at the Institute Pasteur in Paris, National Jewish Centre for Immunology in Denver, and CIBA in Basel, Switzerland.
