Designing Connected Health Systems To Improve Outcomes And Deliver ROI
By Phillips-Medisize Corporation
Mobile and ‘Cloud’ technologies are opening up a number of new service and business models across a range of industries. Using these technologies, new entrant companies have successfully created disruptive business models, capturing existing and new customers and generating strong revenue to grow their businesses.
The biopharmaceutical industry will not be immune to the impact of these new technologies. The applications that are most likely to thrive will be built on two foundations; improving patient outcomes and delivering a strong return on investment for the service provider. Evolving reimbursement practices, which link patient results to payment, help to bring these two pieces together.
This paper explores these themes in more detail, opening the discussion on business models and return on investment (ROI). It is the topic that most industry insiders feel is holding the industry back from significant growth in Connected Health services and solutions.
Improving Patient Outcomes
Healthcare costs are rising globally at an unsustainable level, putting the entire health ecosystem under pressure. Given that there are mounting pressures on the entire system, there is a need to remove inefficiency. One of the largest contributors to preventable healthcare costs is poor prescription adherence - when patients do not take their prescribed medicine as instructed. A recent article in the New York Times referred to this as “an out-of-control epidemic in the United States that costs more and affects more people than any disease Americans currently worry about.”1 Numerous studies have been conducted to measure the level of adherence to medicine prescriptions. The results are alarming. Although the figures vary, most studies indicate only about half of patients take their medication as prescribed. Non-adherence creates significant burden for hospitals; 10% of hospitalizations are caused by non-adherence.2 In the USA alone, this is estimated to cost around $290b, or 2.3% of the annual GDP.3
The evidence suggests that improving adherence will lead to better patient outcomes and will help to control overall healthcare expenditure. An increasing ‘payment for results’ agenda and Accountable Care Organizations are driving a market need for demonstrable outcomes. Numerous disease areas are attracting payers and providers to outcome-based performance measures. This move from activity-based reimbursement to outcome-based reimbursement is already manifesting in requirements for pharmaceutical companies to show real-world evidence and capture Patient Reported Outcome Measures (PROMS).
So, why is adherence so poor, particularly when the benefits are so compelling?
The underlying causes of poor adherence are complex. Patients:
- Forget to take medication or are confused by the prescription
- Don’t think it’s necessary or aren’t feeling better
- Are fearful (needle phobia, potential addiction, see medication as unhealthy)
- Suffer, or fear, side effects
- Struggle to afford the medication costs
- Associate medicine with being ill, not getting better
- Don’t like to depend on drugs
- Discontinue medication when starting to feel better
The truth is that, once a patient leaves a doctor’s office with a prescription, there is almost no way of knowing when, or if, they are taking their medication. When you consider all of the money spent developing life-saving medications, it seems incredibly wasteful that better solutions do not exist to ensure the medication is taken as prescribed.
The good news is that emerging Connected Health technologies provide the opportunity to address and improve patient behavior, particularly when designed with relevant, therapy-specific services that support the needs of the patient and specific medicine treatment(s). A well designed user experience delivers supportive engagement, a great user experience and streamlined data collection and visualization.
In our experience, there is a simple approach to start delivering demonstrable results:
- Define the problem space and opportunity (scope and costs of non-adherence)
- Deploy a monitoring (Connected Health) system as a companion to a therapy-specific device
- Analyze ‘live’ data results to segment the population
- Develop intervention mechanisms tailored to each segment
- Monitor and refine
The long-term goal is to enable patients, supported by their caregivers, to take better care of themselves when in their home and community, and feel equipped to request additional support from healthcare providers (HCP’s) when appropriate. This goal is heavily dependent on the disease area in question. Patients are better equipped to manage their condition when they can see the impact of their treatment. Combining diagnostic measurement with treatment adherence is the ideal. This provides patients with a better ‘cause-effect’ relationship for their medication, and provides HCP’s with a detailed view of condition management and disease progression.
Why a Therapy Specific Device Strategy?
For the patient, Connected Health should be passive and simple. The service design should deliver value on a daily basis and be frequently enhanced to ensure patients remain engaged and motivated. Rewards, such as badges that can be shared with a closed social media group (or publicly if the patient wishes) help gamify the ‘keeping well’ scenario.
This approach enables a more standardized cloud technology that can deliver value across the pharmaceutical company’s enterprise for all franchises and geographies. Uniquely, each patient population can have their own service design and application. At the enterprise level, all data should be collated in a highly structured healthcare database with a proven taxonomy, such as the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), so that global comparators can take place. Thus, it is possible to provide both an enterprise cloud solution and therapy specific devices and apps targeted to patient group needs.
Delivering a Return on Investment (ROI) to the Service Provider
The first question to answer when considering return on investment (ROI) is, who is the investor?
Connected Health systems will not develop themselves. Substantial investment is required to develop, deploy and maintain these systems, particularly within the required regulatory framework in which these systems will need to operate. There are four groups of potential investors: payer organizations, hospitals (healthcare providers), patients (consumers) and pharmaceutical companies. Although all groups are likely to benefit from the successful deployment of such systems, it is unlikely all the groups will provide their share of the initial investment. The payback period for payer organizations is too long term, and fragmented across various systems and schemes.
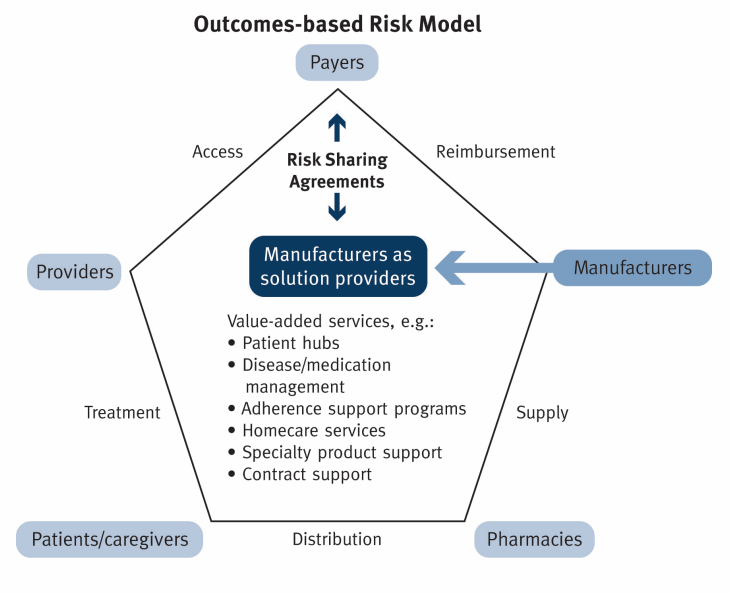
Figure 2: Manufacturers (pharmaceutical companies) as the solution providers, sharing risk payers
For similar reasons, hospitals are not likely investors. The current structure of health care payments makes it difficult to incentivize consumers to invest individually in such systems. This leaves the pharmaceutical companies. With their global reach, long-term outlook, existing incentives to make their drugs successful and the growing trend towards outcome based reimbursement, pharmaceutical companies are the most likely of the investors to define business models that will see solid returns on their initial investments.
Let’s face it though, improving adherence is not sexy. Discovering and launching a new life-saving blockbuster drug attracts far more attention (and funding) in pharmaceutical companies. The ‘blockbuster’ model is a proven method for securing long-term revenue while delivering improved health to society.
Paradoxically, the ‘low hanging fruit’ - improving the patient adherence to treatment - has significant business potential with a relatively high probability for success. In a world where patient preference and payment by results, not activity, are driving changes to healthcare’s business model, pharmaceutical companies can lead these changes, defining a profitable path through this evolving landscape. Great, engaging, service design, including delivery device, apps, analytics and data liquidity, create value. By being the risk bearing entity, pharmaceutical companies can also define the reward structure.
As illustrated in Figure 2 on the previous page, all key players benefit from an increase in patient adherence.
Defining the business case and ROI requires a detailed analysis of revenue and costs. As with any disruptive model, the challenge is that costs appear unavoidably high while revenue is all too uncertain. However, by understanding revenue in terms of nonadherence and controlling costs by focusing on minimal viable products and outsourced services, a strong business case can be established.
The basic parameters to include in the business case will be:
Revenue sources:
- Increased sales based on the increased adherence
- Or reduced decline in the event that generic competitors will enter the segment
- Increase in market share based on improved usability and product differentiation
- Utilizing the Connected Health system to increase the number of patients on the therapy
- Further revenue potential through extended patent protection and provision of additional services across all stakeholders
- Realizing value from the data accumulated
Costs side:
- Investment in Connected Health
- Maintenance and life cycle management
- Device costs (either added to a new device or as an add-on to a current device)
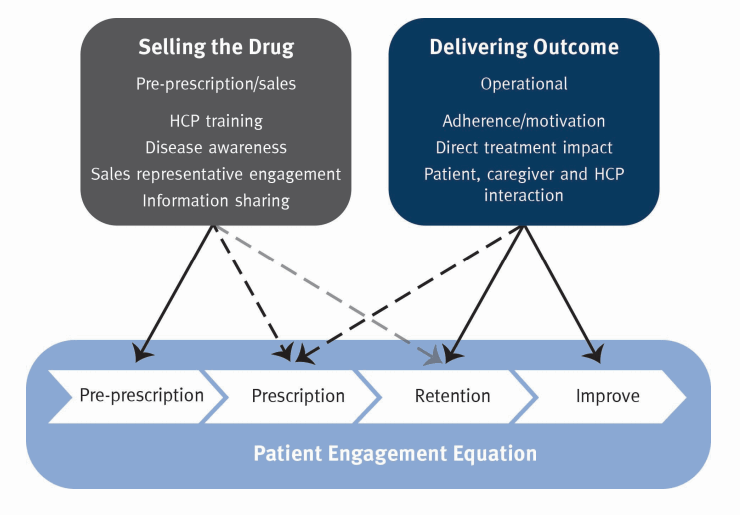
Figure 3: the move from selling the drug to delivering the outcome - Connected Health has a key role to play - and provides both overview of key player interactions and make the business transparent
By building Connected Health into their commercial thinking, pharmaceutical companies will develop a deeper understanding of patient needs and a broader view of value to be added across the full care pathway.
Adopting a holistic and proven approach to Connected Health will help companies improve the patient outcome. This not only provides proven therapeutic benefit, but also better supports patient needs, improves the support provided to patients by other stakeholders, builds a greater understanding of outcome (and how to improve it) and ultimately creates more differentiated products that are highly desired by the full range of users.
1 The New York Times, The Cost of Not Taking Your Medicine, by Jane E. Brody April 17, 2017.
2 Annuals of Internal Medicine 4 December 2012, Interventions to Improve Adherence to Self-administered Medications for Chronic Diseases in the United States: A Systematic Review.
3 Forbes on line article by Tomas Philipson University of Chicago economist, “Non-Adherence in Health Care: Are Patients or Policy Makers Ill-Informed?” May 8, 2015
...
Click here to download the PDF version.
