Risk Mitigation Strategies For Compounding Pharmacy Operations
By Ajay Pazhayattil, Anish Mathew, Marzena Ingram, and Naheed Sayeed-Desta
With the 2018 Compounding Policy Priorities Plan, the FDA has established a clear pathway for advancement of policies for traditional compounding pharmacies and associated outsourcing facilities. The agency intends to implement the strategies while ensuring access to medications for the critical patient population. It is acting under the belief that a growing number of organizations are trying to get into the large drug manufacturers’ domain while operating under pharmacy licenses. The regulator feels there is a significant risk to patients when such organizations start to operate on a large scale. And, Congress backs the FDA’s initiatives to regulate activities that need to adhere to current good manufacturing practices (cGMP). The FDA uses a rigorous abbreviated new drug application (ANDA) approval process for copies of approved drug products. However, the compounding option for such products essentially skips the ANDA process. Compounding pharmacies do not undergo FDA premarket inspections and are subject to nominal quality and compliance rigor compared to biopharmaceutical manufacturing sectors. The FDA has initiated working with state partners to monitor compounding activities.
Let’s examine some major cGMP requirements for sterile manufacturing to get a general understanding of the state of affairs in sterile cGMP manufacturing versus sterile compounding pharmacies. The FDA Guidance for Industry, Sterile Drug Products Produced by Aseptic Processing — Current Good Manufacturing Practice intended to help manufacturers meet the requirements in cGMP regulations (2l CFR parts 210 and 211) when manufacturing sterile drug and biological products using aseptic processing. It applies to an NDA or ANDA or a biologic license application (BLA). The regulator is particular in ensuring the activities are conducted in high-quality environments. In addition to the regular pharmaceutical GMP requirements, the regulations require separate or defined areas of operation in an aseptic processing facility with adequate controls to attain the air quality goals. The area design should satisfy microbiological and particle criteria based on the operational activities conducted in the area. The cleanroom qualification should include assessment of air quality under as-built, static conditions. There is a need for data generated under dynamic conditions (with the personnel present, equipment, and operations performed). The cleanroom classification and operational requirements are very clear. Particle counters must be established to attain meaningful samples, and monitoring must be conducted during regular operation shifts. There is a stress on ensuring minimal product impact during viable and nonviable particle count. HEPA filters with the correct air velocity are required during filling while maintaining a unidirectional airflow pattern. Air pattern analysis needs to be conducted to demonstrate unidirectional airflow and sweeping action. Utilities such as compressed gas should be of appropriate microbiological quality.
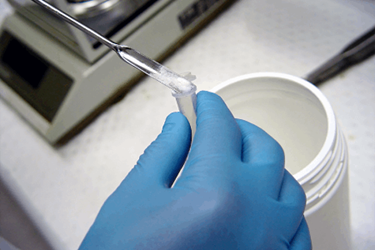
Ensuring applicable aseptic techniques are maintained is another major aspect. It includes moving slowly, keeping out of unidirectional airflow, minimizing manipulations that compromise sterility, sterile materials handling, and maintaining proper gowning controls. Since personnel can be a major contributor to sterile risks, a robust personnel monitoring program involving daily surface samples is a must. Ensuring sterility and integrity of container closure systems is another point of GMP interest. Validation of the sterile filling operations is routinely performed via media fill activities. Here the growth media, such as soybean casein digest media, is exposed to simulated filling operations. The contact surface and exposed growth media is filled and incubated to detect microbial growth. Factors including quantity and number of runs are scientifically justified prior to the study. Worst-case conditions are simulated, including deliberate interventions, per the GMP requirements. Further, each piece of processing equipment is qualified and process operations are validated. Sterility is ensured through the qualification of sterilization process, use of chemical and biological indicators, and monitoring of sterilization process parameters. In cases of sterilization by filtration, filter integrity tests are routinely performed. Routine calibration and preventive maintenance of sterile operating equipment and control instruments are needed. Active environment monitoring and a trending program are also needed. The capability for differentiating identified microorganisms from areas is also a requirement for such operations. Adequate controls and procedures, such as sterility testing, sampling criteria, data integrity, operations recording, and documentation, are required to operate as a sterile GMP manufacturing site.
The FDA has been conducting numerous inspections, has issued more than 180 warning letters to compounding pharmacies, and has initiated recall activities. This in itself highlights the need for a focus on patient safety. Examining a few of the warning letters and 483 observations from 2017 substantiates the regulator’s concerns. In one instance, it was observed that the underside of an aseptic processing work surface was exposed to fiber board with discoloration, indicating microbial risks. Aseptic practices such as disinfecting and cleanroom basic air flow requirements were not being met. And, no studies were performed to demonstrate the bio hoods were qualified for their intended use. In another warning letter, the regulator points to the compounder failing to disinfect equipment prior to use in aseptic operations. Media fills were not conducted to challenge the conditions, and smoke studies could not adequately demonstrate the room was capable of providing adequate product protection. In one 483, it was observed that the technicians used nonsterile booties, hairnets, masks, and gowns while going into a cleanroom with laminar airflow hoods (LAFHs). A compounder failed to investigate product failures. Expired cleaning agents were used in another instance. In certain cases, there was no environmental monitoring. In one instance, the regulator stated the firm lacked scientific justification for using the sterilization validation method for compounded pellet products. In certain cases, products that failed to meet specifications were not rejected. The lack of employee training was reflected in multiple regulator observations. Containment, segregation, and cleaning requirements of hazardous drugs were not considered by some organizations.
Procedural and documentation deficiencies were rampant throughout the warning letters and 483s. All of this introduces major product contamination risks during compounding. The concerns listed are considered the basic necessities of a commercial sterile biopharmaceutical manufacturing operation, and such violations are considered lack of basic aseptic cGMP requirements. The observations discussed above are just from 2017. The consistent, gross violation pattern observed within the compounding pharmacy sector points toward the need for a fundamental shift.
Compounding pharmacy activities are here to stay, as they are a clear patient and physician treatment need. However, this is the time for compounding pharmacies to make strategic operational decisions. The switch from pharmacy-based operations to absolutely contained aseptic cGMP operations incurs substantial investments. Current innovations in cleanroom technologies and single-use systems open up major opportunities for organizations willing to upgrade to regulatory-compliant technologies. However, the sector lacks the expertise in identification, selection, qualification, and commissioning of such innovations with smaller footprints. It calls for existing commercial biopharmaceutical engineering, qualification, and GMP regulatory consultants to step up and offer tailored solutions for the compounding industry. With the regulator focus on streamlining compounding operations, an initial gap assessment will be the first step, followed by developing a detailed project plan. Implementing a regulatory risk-free compounding operation also comes with the need for specific employee training and the addition of scientific capability and rigor. The existing talent pool within the biopharmaceutical industry holds transferrable skills fit for compounding operations.
The FDA has substantial expertise in oversight of commercial biopharmaceutical sterile manufacturing operations. The regulator’s expertise is reflecting in the guidances, observations, and 2018 Compounding Policy Priorities Plan. The FDA guidance for industry on Compounded Drug Products That Are Essentially Copies of a Commercially Available Drug Product Under Section 503A of the Federal Food, Drug, and Cosmetic Act and the guidance for industry on Compounded Drug Products That Are Essentially Copies of Approved Drug Products Under Section 503B of the Federal Food, Drug, and Cosmetic Act are the first steps. Per FDA Commissioner Scott Gottlieb, the plans and commitments on compounding pharmacy operations are targeted to be finalized by 2018. The regulator’s high level of focus and the availability of biopharma expertise and technologies make it prime time for existing compounding organizations to think about a business transformation. Waiting for regulatory action may result in major operational disruptions. The opportunity exists for organizations with long-term growth objectives, as the continued regulator focus may trigger consolidation and minimize the number of compounding operations.
Note: This article was prepared by the authors in their personal capacity. The opinions expressed are the authors’ own and do not reflect the view of their employers, governments, or any agencies with which they are affiliated.
References:
- https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm121568.htm
- https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/PharmacyCompounding/ucm339771.htm
- https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/PharmacyCompounding/ucm592795.htm
- https://www.fda.gov/NewsEvents/Newsroom/FDAInBrief/ucm592610.htm
- https://www.fda.gov/downloads/Drugs/Guidances/ucm070342.pdf
- https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM510153.pdf
- https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM510154.pdf
About The Authors:
 Ajay Babu Pazhayattil, M.Pharm, has held key management roles with brand name, generic, and contract manufacturing organizations. He is an industrial pharmacist with experience in multiple segments of pharmaceutical operations. Pazhayattil has extensive experience conducting global GMP audits and has conceived, implemented, and promoted novel technology innovations based on sound scientific principles. His experience extends through solid-dose, liquids, and small and large volume parenteral dosage forms. Pazhayattil is involved with industry organizations and has published multiple journal articles.
Ajay Babu Pazhayattil, M.Pharm, has held key management roles with brand name, generic, and contract manufacturing organizations. He is an industrial pharmacist with experience in multiple segments of pharmaceutical operations. Pazhayattil has extensive experience conducting global GMP audits and has conceived, implemented, and promoted novel technology innovations based on sound scientific principles. His experience extends through solid-dose, liquids, and small and large volume parenteral dosage forms. Pazhayattil is involved with industry organizations and has published multiple journal articles.
 Anish Mathew, M.Pharm, R.Ph., has operated chain, independent community, and compounding pharmacies across Florida for over a decade. He has contributed to academia as assistant professor in pharmacology as well as in the clinical pharmacy field. He has expertise in compounding different pharmaceutical dosage forms.
Anish Mathew, M.Pharm, R.Ph., has operated chain, independent community, and compounding pharmacies across Florida for over a decade. He has contributed to academia as assistant professor in pharmacology as well as in the clinical pharmacy field. He has expertise in compounding different pharmaceutical dosage forms.
 Marzena Ingram is a pharmaceutical industry professional with extensive quality assurance and technical operations experience; she holds a senior management position. Ingram developed a specialized continued process verification team and spearheaded the implementation of a product life cycle program to meet global regulatory requirements. She also introduced statistically driven product assessment processes and led the implementation of a comprehensive life cycle management software solution. Ingram has authored multiple pharmaceutical journal articles.
Marzena Ingram is a pharmaceutical industry professional with extensive quality assurance and technical operations experience; she holds a senior management position. Ingram developed a specialized continued process verification team and spearheaded the implementation of a product life cycle program to meet global regulatory requirements. She also introduced statistically driven product assessment processes and led the implementation of a comprehensive life cycle management software solution. Ingram has authored multiple pharmaceutical journal articles.
 Naheed Sayeed-Desta has been responsible for providing strategic directions on life cycle management for over 300 active solid-dose products. Sayeed-Desta champions delivery of science- and risk-based approaches from traditional to novel manufacturing technologies. She is a proven leader in pharmaceutical manufacturing science and technology. Her expertise in providing pragmatic solutions for manufacturing operations is well recognized. She has been the lead author of journal articles. Sayeed-Desta is also an active contributing member of pharmaceutical industry organizations
Naheed Sayeed-Desta has been responsible for providing strategic directions on life cycle management for over 300 active solid-dose products. Sayeed-Desta champions delivery of science- and risk-based approaches from traditional to novel manufacturing technologies. She is a proven leader in pharmaceutical manufacturing science and technology. Her expertise in providing pragmatic solutions for manufacturing operations is well recognized. She has been the lead author of journal articles. Sayeed-Desta is also an active contributing member of pharmaceutical industry organizations
