Is Biopharma's Response To Coronavirus Off The Mark?

By Matthew Pillar, Editor, Bioprocess Online
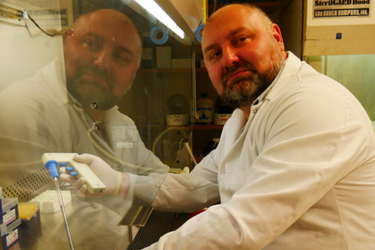
As biopharmas aplenty race to develop a vaccine, CureLab’s Alex Shneider says an incorrect approach risks turning the currently insignificant coronavirus threat into a deadly pandemic. He suggests that we should instead be focused on the development of adjuvants and immunostimulants to protect the elderly.
If the collective biopharma pipeline is any indicator, we are about to witness an epic battle for dominance on the coronavirus vaccine front as numerous companies race for the earliest release. To name a few, CureVac, GlaxoSmithKline, Inovio, Johnson & Johnson, Moderna, and Sanofi represent just a small sampling of the big players of vaccine production. As it currently stands, Moderna’s candidate, mRNA-1273, is in first place. Now at Phase 1, the company identified the candidate a mere 42 days after COVID-19 was sequenced.
While he doesn’t discount the gravity of the virus’ global assault, CureLab founder and CEO Alex Shneider is more than a bit dismayed at the extraordinary effort to produce its vaccine. In fact, he does not mince words when he tells me, verbatim, that “the current attempt to produce a vaccination could have a disastrous effect.”
This statement alone may be shocking, but Shneider offers some historical context to support his suspicion. Some of his colleagues in epidemiology believe this to be the fifth such episode in recorded human history. “One was roughly 800 years ago. One was around 200 years ago. One was roughly 120 years ago. Another was roughly 70 years ago. The more I talk to people who have studied the history of these viruses, the less reason I see to be panicky,” he says.
Further, Shneider’s colleague Andrey Komissarov, PhD, who heads the lab of molecular virology at the WHO-recognized National Influenza Center in St Petersburg, asserts that a coronavirus—though not the COVID-19 strain—has been constituting about 2 percent of respiratory infections in Russia for the past several years. Furthermore, Shneider is certain that the same rate would also be observed in other countries too, should the proper retrospective analysis be conducted. “It's not that it didn't exist in a population and now, suddenly, we started recording cases,” says Shneider. “It became a subject under the magnifying glass of disproportional coverage. I believe that a retrospective analysis of respiratory-related hospitalizations for previous years is urgently needed to calm this hysteria down. I predict that it would demonstrate that some level of coronavirus patients, similar to the current incidence rate, was here all this time while causing no panic.”
That retrospective analysis, he contends, would support his assertion that the life science community’s resources in the coronavirus battle should instead be focused on the development of immunostimulants and adjuvants to protect the elderly population most afflicted by the disease.
The wrong vaccine can turn a mild problem into an unprecedented pandemic tragedy.
To be clear, Shneider is a scientist, not an anti-vaxxer. He celebrates the practical eradication of smallpox, polio, and other diseases as examples of vaccines succeeding. He served as a section editor in the International Reviews of Immunology and, in addition to his corporate work, holds academic appointments.
To make his case, Shneider reverts back to the fundamentals of innate and adaptive immunity. “Innate immunity is demonstrated when you cut your finger and your immune system indiscriminately attacks whatever is getting in without regard to the antigen. Adaptive immunity determines and attacks a particular antigen,” he explains. “Further, there are two types of adaptive immunity: B cell and T cell. In the case of many vaccines, B cells are triggered to produce antibodies which bind to freely floating viruses, bacteria, or toxins with the goal of eliminating them from the body.”
While this strategy is often overwhelmingly effective, Shneider fears that coronavirus might utilize uncommon tactics called “antibody-dependent enhancement,” present in some viruses, hijacking the body's antiviral immune response and turning it into its own advantage. “Some viruses adopt a strategy to use antibodies against themselves to expedite and enhance the infection,” he says. “It seems that, unlike flu, coronavirus can infect the same person multiple times during the course of a singular season. This, as well as other factors, may indicate that it’s using the antibodies against the virus to expedite and enhance the infection,” he says. “While the hope of the B cell vaccine is to equip the body with coronavirus antibodies, there’s a very real possibility that we’ll, in fact, be inadvertently equipping the virus. Now, imagine what would happen if we vaccinate millions of people this way, making them perfect targets for the viral attack.”
“We may take a minor threat and make it a colossal threat of a historical proportion.”
-Alex Shneider, Founder & CEO, CureLab
“The risk, when weighed against the relatively mild nature of the virus (the elderly and immunocompromised notwithstanding), is too high,” he says. “We may take a minor threat and make it a colossal threat of a historical proportion,” says Shneider. He points out previous attempts at the HIV vaccine that, in fact, exacerbated the danger of the disease.
Furthermore, he believes that this danger is further aggravated by the fact that it may be impossible to truly test the vaccine protective potency, as it would take too long and require too many study participants. Thus, it is exceedingly likely that regulators will greenlight an anti-coronavirus vaccine based solely on the criteria that the vaccine is not in-and-of-itself toxic, and induces surrogate markers of the antiviral immune response.
T cell immunity, on the other hand, does not focus on a freely floating passenger. Instead, it aims to recognize cancerous or infected cells, destroying and eliminating them from the body so they cannot propagate or generate new viral particles. Shneider doesn’t discount the potential of a T cell vaccine. “Coronavirus, it seems, mutates significantly less than flu. Thus, it’s a much easier vaccine target.” For example, the largest protein in the virus is RNA-dependent RNA polymerase, which is evolutionarily conserved and unlike anything in the human genome. “It may be a good strategy to develop T cell vaccines against cells which express these viral genes because these cells, unless they express this gene contracted from a DNA vaccine, would only have it because the virus is present in the cell,” he says. Shneider notes, however, that it’s early days for T cell vaccines and the data is a bit thin to date. Even more so, he believes that although creating a T-cell vaccine against coronavirus may be a relatively easy task, this vaccine will most likely serve little to no purpose.
If Effective, Who Would The Vaccine Protect?
As he considers the potential risks and benefits of a coronavirus vaccine, Shneider again invokes influenza. “The question is not how will we win over flu, or coronavirus,” he says. “The question is, how long can we wait until they become much more tragic problems than they are today?”
Our aging population is a key consideration in the answer to that question. The elderly population, coupled with flu and new novel viruses like COVID-19, creates a historically unparalleled situation. And the science community, he contends, is not adapting to that situation appropriately.
“Elderly people do not react to vaccination the same way young people do,” says Shneider. “And yet, how do we test vaccines? Using young mice, young rats, young ferrets. When the vaccine comes to market, who will it be good for? Young people. Young people are not the ones predominantly dying from Coronavirus.”
The Need For Adjuvant/Immunostimulant Therapy for the Elderly
Generally speaking, a vaccine consists of two major elements: an antigen the vaccine is targeted against and an adjuvant which makes a vaccine work effectively. Shneider is calling on the life sciences community to allocate resources to the development of adjuvants and immunostimulants to protect the population most vulnerable to these viruses—the elderly. He says we need to stop spending so many resources on a viral antigen for a vaccine that, ultimately, is not very problematic—and instead focus our resources on protecting the elderly from this and many other viral threats to their health. More specifically, until we address chronic inflammation in the elderly, we can continue to expect poor vaccine protection and a compromised immune response among that population.
Interestingly, Shneider says he’s hearing a lot of scientific crosstalk between virology and vaccinology not just in the context of coronavirus, but also in other areas of biomedical science including cancer and diseases of chronic inflammation. “Coronavirus is a wake-up call not for vaccine development in the context of this particular virus, but for creation of long-overdue adjuvants and therapies for chronic, immunocompromising conditions in the elderly.”
Why, Then, Are We Rushing Toward A Coronavirus Vaccine?
“In a phrase, mental inertia,” says Shneider. That’s roughly defined as: The basis that prevents a scientist from taking the most productive steps and the most adaptive reasoning available with the current level of scientific methods, approaches, and techniques. Shneider even wrote a paper on the subject a while back. Many of its takeaways apply equally to the mainstream media which, once it gained a head of steam, made no apologies for whipping the world into an exaggerated frenzy over the virus. “Overreaction by the media—and the potential that we’ll see a boy-who-cried-wolf scenario play out when a more serious global health threat does arise—is a more existential and long-term public health threat than this virus,” he says.
We’ve already ascertained that Shneider is no anti-vaxxer. He’s also no conspiracy theorist, although, if taken out of context, his pragmatic take on the beneficiaries of coronavirus might be interpreted as such. In a recent email to me, he wrote:
“Although I am absolutely certain that COVID-19 happened naturally and no ill will played a role… Before the situation went out of control, the way the story was used promised to be good for the Chinese because they won’t have to implement the pledge they made Trump to purchase American goods for hundreds of billions of dollars. In the long term, it’s good for American industry because now it will have a justifiable reason to get off the Chinese manufacturing needle. It was good for Democrats because the inevitable spread of the infection through the American population, combined with the stock market crash, gives them new ammunition to use in the upcoming general election. It was good for Republicans because now people finally see that controlling the border is necessary to prevent the uncontrollable spread of infections. It was good for academia because it brings more funding to their labs. It was good for the bureaucracy because it can create a new regulatory apparatus, which guarantees more staff and governmental resources. It may be good for global peace because instead of fighting each other, we need to unite to fight the infection, which knows no borders. After all, it was the Spanish flu which partially stopped WWI. It’s good for the media because it creates a spike in news interest.”
“Well,” he concluded his email, “perhaps, it’s not good for common people. But, who ever cared about common people?”
